Navigating the preclinical and clinical years and how you landed on your specialty, and things worth considering?
Medical school is essentially split into two sections: preclinical and clinical years. Over the course of these four years, you are expected to decide on a specialty that you can see yourself enjoying for the next 20-30 years. What happens during your preclinical years? What happens during your clinical years? How am I supposed to decide on a lifelong career in less than four years? As I take you all through my experience through medical school, I will be sure to touch on all these questions, along with some other important points to consider.
Preclinical years:
Preclinical years are traditionally 2 years in length, but several medical schools are switching to 18 months of preclinical time. Pre-clinical means exactly what you would think: it is the period before you begin clinical rotations. This section of medical school looks very similar to your undergraduate years, with much of your time being spent in the classroom. Though there is some variation from one medical school to another you have more control over how you take in the information being presented. While some med schools require you to attend classes in person, others allow you to watch lectures live, watch them at a later date, and some med schools have all these options available for you to choose from.
Personally, I consider myself a disciplined person; I also consider myself to be a morning person. With this in mind, I decided not to attend any lectures during my preclinical years, and I woke up at 4am to begin studying. I would essentially teach myself the lectures for the day and then watch the recorded lectures that evening. This allowed me to make the necessary connections on my own, then listen to my professors teach it to me. I was able to get more out of lectures by already going through them in depth beforehand.
Preclinical tips:
#1 Be sure to know YOURSELF! If you are someone that does better with having structure and going to lecture, then you
DO NOT need to be studying at home. If you are a night owl, you DO NOT need to be trying to wake up early to study.
#2 Med school is not the time to try to reinvent yourself. Work to your strengths — after all, they are what got you accepted to medical school, which is no easy feat!
Clinical years:
In my opinion, the clinical years is when all the fun begins.
During this time, you will rotate through nearly every specialty in medicine. You will begin rotations with little expectations. As you progress through your 3rd year you will be expected to take on more responsibilities with your patients, as well as come up with more comprehensive treatment plans. Among the biggest things that will be expected of you is to know your patients very well! Med students do not carry as many patients as residents or attendings; due to having less patients you are expected to know so more about each of them. During 4th year you will begin preparing yourself for your intern year! With that you will begin to take on even more responsibilities, patients and the alike. The goal is to get as close as you can to an intern workload.
Clinical tips:
#1 Arrive on time every single day! There are many things out of your control but being timely is not one of them.
#2 Know your patients better than anyone else on your service. HPI, PMH, FamHx, etc, no one should know more than you.
#3 Be sure to stay organized with your thoughts and clinical presentations.
How to choose a specialty:
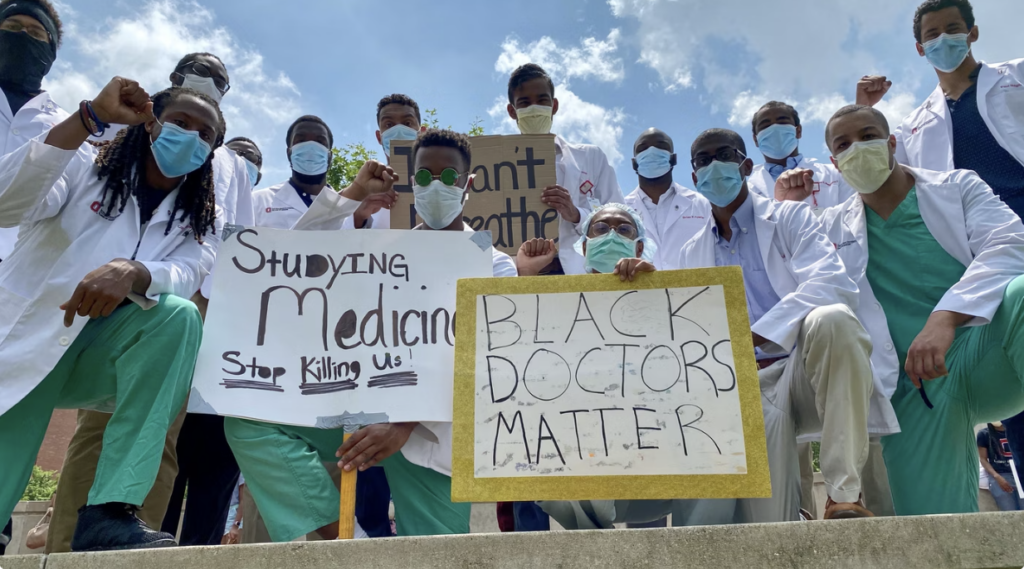
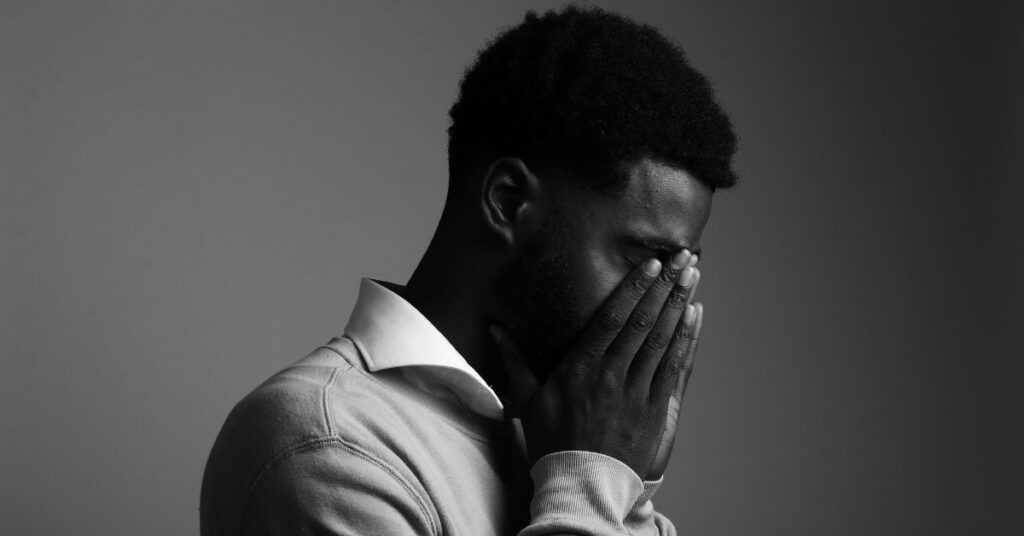
Physician depression, suicide and burnout are all higher than the general population. Choosing the right specialty for you can go a long way in mitigating the likelihood of this occurring. There are several aspects people look at when choosing a specialty: prestige, salary, lifestyle, the people in that field, etc. In my opinion, neither of those are the most important. Your true genuine interests should remain paramount in your decision!
At the very “worst,” as a physician you will command a $250,000 salary – that is a lot of money! A lot of medical students make the mistake of comparing salaries within specialties. If you want to compare salaries, you should do it against the average American household income, which is around $50,000. So, basically, a “low paying specialty” will make FIVE TIMES more than the average American household. Regardless of specialty, physicians are in the top 5% of all income earners in the US, meaning the lowest paying physician still makes more than 95% of Americans. Also, this isn’t even considering if your spouse is working.
There is no amount of money that will satisfy you from spending time with your family, enjoying your hobbies, or going to a job that you don’t truly enjoy. This is especially true after you’ve made a quarter of a million dollars or more for 5, 10, 15+ years. My entire life I have witnessed firsthand people going to a job they don’t enjoy, so this is particularly important to me. There is nothing I want to see more than BMIM truly thriving and truly happy in their careers, and not just social media “thriving and happy.”
People commonly talk mention figuring out of you’re a “surgical” or “medicine person.” Though I didn’t initially believe in this, I think it’s a good starting point. Until I started my clinical years, I thought I was a surgical person. I kept an open mind and truly explored every specialty and found out that I am much more of a medicine person. I would not have been able to figure that out if I didn’t keep an open mind and follow my interests, and not money and prestige.
Specialty tips:
#1 Don’t chase salary, you will make more than enough over your career regardless of specialty.
#2 Don’t chase prestige, other people’s opinion of your career will not mean much when you’re not able to do the things you enjoy or go to a job that truly fulfills you.
#3 Do chase your interests, as you will reap the benefits of working in a field that you enjoy in your personal and professional life for years to come!